What Is T1D?
Type 1 diabetes (T1D) is a chronic autoimmune disease where the pancreas produces little to no insulin, the hormone responsible for regulating glucose levels in the blood. Inside the pancreas are islets of Langerhans, clusters of different cell types that play significant roles in regulating metabolism. The most common is the beta cell, producing the hormone insulin when triggered by natural spikes in blood sugar. Insulin is responsible for ‘opening the door’ to the body’s cells, allowing glucose to exit the bloodstream and enter different cells that cycle it into energy.
For someone in the T1D community, these insulin-producing beta cells are attacked by T-cells sent from the body’s immune system. Beta cells are then killed off, unable to produce insulin.
What Happens When the Body Can’t Produce Insulin?
When beta cell mass is depleted, glucose is trapped and builds up in the bloodstream. Doors to the body’s cells are welded shut, starving them of energy. Without insulin to open these doors, the body will begin to break down its own fat and muscle in a final attempt to get energy, leading to high blood sugar and, if left untreated, life-threatening diabetic ketoacidosis (DKA).
What Is the Difference between Type 1 and Type 2 Diabetes?
Type 1 diabetes is a lifelong condition caused by the immune system attacking its healthy insulin-producing beta cells so the body cannot regulate blood sugar levels. T1D does not have an exact cause and is not preventable or curable. T1D requires external insulin injections for the rest of the patient’s life, calculated alongside the current blood glucose level to ensure the right amount of medication is given to prevent high (hyperglycemia) and low (hypoglycemia) blood sugars.
Type 2 diabetes occurs when the pancreas can make insulin unhindered, but the body is insulin resistant and no longer responds to the hormone as it once did. An estimated 96% of global cases of diabetes are type 2. The body will try to overcompensate by producing more insulin, but the patient may eventually need external insulin. T2D is caused by lifestyle and environmental factors, with heightened risk in those with a family history. Patients can impact the trajectory of their T2D diagnosis with changes in diet and exercise, and in some cases, can reverse the disease after onset.
What Are the Stages of T1D?
Stage 1
The first stage is marked by the presence of two or more islet autoantibodies. These autoantibodies are proteins triggered by the beginning of an immune response only seen in T1D. At this stage, an individual displays normal blood sugar levels and no outward signs that something is wrong. Over 95% of people with new-onset T1D will have at least one detectable islet autoantibody. The risk of developing T1D at this stage is 44% within the next five years and 70% within the next 10 years. The lifetime risk is nearly 100%.
Stage 2
In this stage, people begin to experience higher blood sugar levels than normal. The pancreas is still working to produce insulin. Although production is weaker, it is often not enough to outwardly signal symptoms of T1D. Insulin is not yet needed.
Stage 3
Most T1D diagnoses occur at this stage because the symptoms are so pronounced. Beta cells are now under full attack by the immune system and unable to produce enough—or any—insulin to keep up with the body’s needs. Glucose is not broken down by insulin and instead stays in the bloodstream. The high blood sugar levels cause unexplained weight loss, frequent urination, exhaustion, flu-like symptoms, and more. Insulin therapy is immediately needed from this point onward. Prolonged high blood sugar levels lead to DKA, where the body converts its own fat and muscle into energy, releasing acidic ketones that are life-threatening. It is estimated that 30-46% of T1D children have DKA at diagnosis.
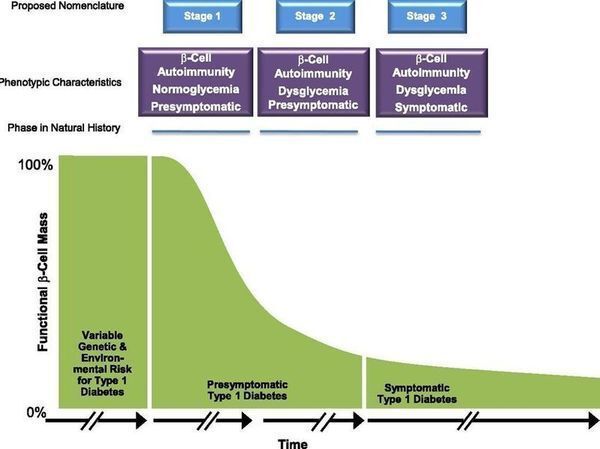
Insel, Richard A., et al. “Staging Presymptomatic Type 1 Diabetes: A Scientific Statement of JDRF, the Endocrine Society, and the American Diabetes Association,” Diabetes Care 38, no. 10 (2015): 1964–74. https://doi.org/10.2337/dc15-1419.

